HPV Vaccine Protecting Against Cancer
Vacuna virus papiloma humano is crucial for preventing cervical cancer and other HPV-related diseases. This comprehensive guide explores the science behind this life-saving vaccine, delving into its efficacy, safety, and the broader public health impact it has.
From understanding the different types of HPV and their potential health risks to exploring vaccination strategies and the role of healthcare providers, this resource provides a thorough overview of the critical aspects surrounding HPV vaccination. We also touch on the global perspective and challenges faced in implementing these programs worldwide.
Introduction to HPV Vaccine
The human papillomavirus (HPV) is a common sexually transmitted infection (STI) that can cause various health problems, including genital warts and certain cancers. Understanding HPV and its implications is crucial for proactive health management and preventing severe consequences. This blog post delves into the basics of HPV, its different types, the importance of vaccination, and the history and development of available vaccines.HPV is a group of more than 200 related viruses.
Most HPV infections are harmless and resolve on their own, but some types can persist and lead to serious health issues. The virus is primarily transmitted through skin-to-skin contact, often during sexual activity.
Getting vaccinated against the HPV virus is crucial for health, and it’s great to see politicians like Biden stepping up and prioritizing infrastructure projects, like those discussed in the recent article taking on trump biden promotes infrastructure decade in wisconsin. Stronger communities and better healthcare go hand in hand, making sure everyone has access to preventative measures like the HPV vaccine is a win-win for the future.
Understanding HPV Types
Different HPV types have varying degrees of risk. Some cause benign conditions like genital warts, while others are linked to cancers of the cervix, vagina, vulva, penis, anus, and oropharynx (the back of the throat). Certain high-risk HPV types are responsible for a significant proportion of these cancers.
Health Implications of HPV Infection
The health implications of HPV infection range from mild to severe. Genital warts are a common manifestation of HPV infection, often appearing as small, fleshy growths in the genital area. However, the most concerning implication is the link to various cancers. Persistent infections with high-risk HPV types can lead to cellular changes that, if left untreated, can develop into cancerous tumors.
For example, cervical cancer, a leading cause of cancer-related deaths in women, is strongly associated with persistent infection with high-risk HPV types.
Importance of HPV Vaccination
Vaccination against HPV is a crucial preventative measure. The vaccine significantly reduces the risk of developing HPV-related cancers and genital warts. Vaccination is particularly important for young people, as it protects them before they are exposed to the virus. Early vaccination offers the best protection and can potentially prevent serious health issues later in life.
Historical Context of HPV Vaccine Development
The development of HPV vaccines was a significant advancement in public health. Early research focused on understanding the virus and its role in causing various diseases. Subsequent efforts led to the creation of vaccines that effectively target high-risk HPV types. This research spanned several decades, involving numerous scientific collaborations and rigorous clinical trials. For instance, the development of the Gardasil vaccine, a pivotal moment in HPV prevention, involved extensive research and trials to ensure its safety and efficacy.
Available HPV Vaccines and Their Characteristics
Several HPV vaccines are available worldwide, each with its own benefits and drawbacks. These vaccines primarily target high-risk HPV types associated with cancers.
Thinking about the HPV vaccine lately, and it got me pondering the complexities of public health decisions. While preventative measures like the HPV vaccine are crucial, it’s interesting to consider how the recent verdict in the Trevor Bickford terrorist attack guilty case trevor bickford terrorist attack guilty highlights the need for a balanced approach to public safety.
Ultimately, understanding the long-term impact of the HPV vaccine on future generations remains a priority in public health campaigns.
- Gardasil: This vaccine protects against several high-risk HPV types, including those that cause cervical cancer and genital warts. It is generally well-tolerated with minimal side effects.
- Gardasil 9: This is a newer version of the Gardasil vaccine, providing protection against nine high-risk HPV types, including additional types not covered by the original Gardasil. This expanded coverage is a significant advancement in preventing a broader range of HPV-related cancers.
- Cervarix: This vaccine protects against two high-risk HPV types, which are the main types causing cervical cancer. While effective, its coverage is narrower compared to Gardasil and Gardasil 9.
These vaccines are generally administered in a series of injections over several months. The optimal age for vaccination is typically during pre-teen and teenage years, before exposure to the virus. Individuals can discuss the suitability of the vaccine with their healthcare providers.
Getting vaccinated against the HPV virus is super important, and it’s something I’m always passionate about. Speaking of important things, did you see all the stunning photos from the Critics Choice Awards red carpet? critics choice awards red carpet photos It’s so cool to see celebrities looking their best, and it totally reminds me why preventative health, like HPV vaccination, is so crucial for everyone.
Protecting yourself against potential health issues is just as important as admiring great style.
Vaccine Efficacy and Safety
The human papillomavirus (HPV) vaccines have proven to be a crucial tool in preventing cervical cancer and other HPV-related cancers. Understanding their efficacy and safety is paramount for informed decision-making regarding vaccination. Rigorous scientific studies and extensive monitoring programs have provided compelling evidence supporting their use.This section delves into the robust scientific backing behind HPV vaccine efficacy, examines the extensive long-term safety data, and compares the profiles of different vaccines.
It further Artikels potential side effects, their frequency, and the comprehensive monitoring procedures in place to ensure continued safety.
Scientific Evidence Supporting Efficacy
The efficacy of HPV vaccines is well-established through extensive clinical trials. These trials have demonstrated that HPV vaccines are highly effective at preventing infection with the targeted HPV types. The vaccines work by stimulating the immune system to produce antibodies that neutralize the virus, preventing it from causing infection and subsequent cellular damage.Observational studies further support the efficacy of HPV vaccines in reducing the incidence of HPV-related diseases, including cervical cancer.
These studies have shown a clear correlation between vaccination rates and a decline in the prevalence of specific HPV types in vaccinated populations.
Long-Term Safety Data
Long-term safety monitoring of HPV vaccines has consistently demonstrated their safety profile. Millions of individuals have received these vaccines worldwide, and the data collected from these large-scale vaccination programs show a low rate of serious side effects.The vast majority of reported side effects are mild and transient, such as pain at the injection site, fever, or fatigue. Notably, no significant long-term adverse health consequences have been linked to HPV vaccines.
This safety record, reinforced by ongoing surveillance, is crucial for public confidence in the vaccine.
Comparison of Efficacy and Safety Profiles of Different HPV Vaccines
Different HPV vaccines vary slightly in their targeted HPV types and formulations. Cervarix, for example, protects against HPV types 16 and 18, which are responsible for a large proportion of cervical cancers. Gardasil, on the other hand, protects against a broader range of HPV types, including types 6 and 11, which cause genital warts. The efficacy and safety profiles of these vaccines are comparable, with both demonstrating high efficacy and a low incidence of serious side effects.
Potential Side Effects and Frequency
Common side effects associated with HPV vaccines are generally mild and include pain, redness, or swelling at the injection site, fever, headache, and fatigue. These side effects typically resolve within a few days. Serious side effects are rare and include allergic reactions. The frequency of these side effects is low, aligning with the safety profiles of other vaccines.
“Data from large-scale vaccination programs indicate a very low incidence of serious side effects.”
Monitoring Procedures for Vaccine Safety, Vacuna virus papiloma humano
Extensive monitoring programs are in place to track and assess the safety of HPV vaccines. These programs include ongoing surveillance systems that collect data on potential adverse events following vaccination. This data is meticulously analyzed to identify any potential safety concerns and to ensure the vaccines remain safe for use.Independent safety review boards continuously evaluate the safety data and provide recommendations for the use and monitoring of HPV vaccines.
This comprehensive approach to safety monitoring provides confidence in the continued use of these life-saving vaccines.
Target Populations and Vaccination Strategies
The HPV vaccine is a crucial tool in preventing cervical cancer and other HPV-related cancers and diseases. Understanding the recommended target populations and vaccination strategies is vital for maximizing its impact and achieving herd immunity. This section delves into the specific age groups benefiting from vaccination, the importance of vaccinating both boys and girls, and strategies to boost vaccination rates within different demographics.
We’ll also explore the critical role healthcare providers play in ensuring HPV vaccination programs are effective.
Recommended Age Groups for HPV Vaccination
The optimal time for HPV vaccination is typically during adolescence, before exposure to the virus. This preventative measure allows the body to develop immunity before potential infections occur. The most effective time frame is generally between the ages of 11 and 12 years old, although it can be administered as early as nine years old. Vaccination can also be administered up to age 26 for those who have not been vaccinated previously.
Importance of Vaccination for Both Boys and Girls
HPV is a sexually transmitted infection, and both males and females can be infected. HPV infection can lead to various health problems, including genital warts, cancers of the cervix, vagina, vulva, penis, anus, oropharynx, and more. Vaccinating both boys and girls protects both sexes from the virus and its associated health consequences. This comprehensive approach is crucial for promoting overall public health.
Strategies for Increasing Vaccination Rates in Different Populations
Boosting vaccination rates involves addressing various factors, including cultural beliefs, access to healthcare, and financial constraints. Strategies include community outreach programs, educational campaigns, and partnerships with community leaders to dispel myths and highlight the benefits of vaccination. Government initiatives, insurance coverage, and convenient vaccination locations can also play a vital role in increasing accessibility and uptake. In areas with lower vaccination rates, targeted campaigns focusing on specific communities can be very effective.
Role of Healthcare Providers in Recommending and Administering HPV Vaccines
Healthcare providers play a critical role in recommending and administering HPV vaccines. They should provide comprehensive information about the benefits, risks, and side effects of the vaccine. Clear communication and addressing any concerns can help build confidence and encourage vaccination. Providers should also ensure the vaccine is administered according to the recommended schedule. This includes discussing vaccination options with patients and their families, especially in situations where parents or guardians have reservations.
Thinking about the HPV vaccine? It’s a crucial preventative measure, but sometimes navigating the complexities of workplace issues can feel just as challenging. For example, if you feel like an employer, like Budget, improperly handled a situation regarding your phone, and you have proof, you might want to check out this story about a similar situation: help an employee of budget kept my phone and i can prove it.
Ultimately, prioritizing your health and well-being, including getting vaccinated against HPV, should always be a top priority.
Regular training for healthcare providers on the latest recommendations and best practices is also crucial.
Vaccination Schedules for Different Age Groups and Vaccines
The following table summarizes the recommended vaccination schedules for various age groups, including the different HPV vaccines available. Note that specific schedules may vary based on the specific vaccine product used.
| Age Group | Vaccine Type | Schedule |
|---|---|---|
| 11-12 years | Cervarix, Gardasil, Gardasil 9 | Two doses, typically 6-12 months apart |
| 15-26 years | Cervarix, Gardasil, Gardasil 9 | Three doses, typically 0, 1-2, 6 months |
| Previously unvaccinated 15-45 years | Gardasil 9 | Two or three doses depending on prior vaccination status. Consult a healthcare provider for specific recommendations |
Public Health Impact and Global Perspective
The human papillomavirus (HPV) vaccine has emerged as a crucial tool in global public health, demonstrating significant potential to prevent a multitude of cancers and other HPV-related diseases. Its implementation has shown promising results in reducing the burden of these illnesses, highlighting the importance of widespread vaccination programs. However, challenges remain in ensuring equitable access and comprehensive coverage in all regions.Understanding the global impact of HPV vaccination requires a comprehensive view of its effectiveness, the prevalence of HPV-related diseases, and the challenges associated with its implementation.
This section explores the positive public health outcomes, examines regional variations in disease prevalence, discusses strategies for vaccine implementation, and highlights the critical role of international collaborations in ensuring global impact.
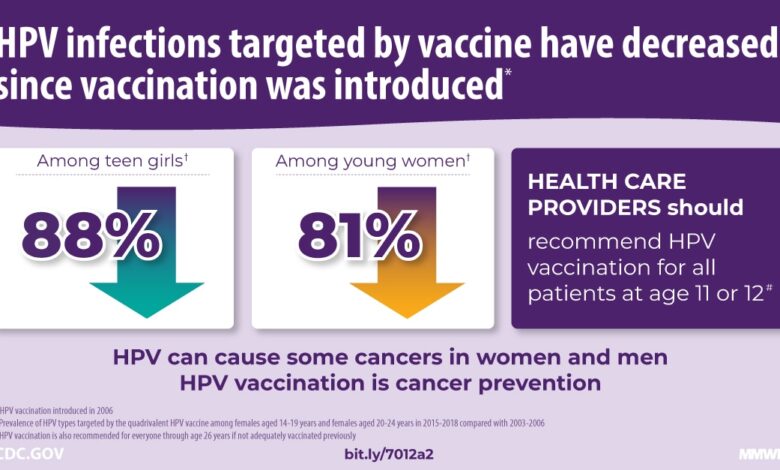
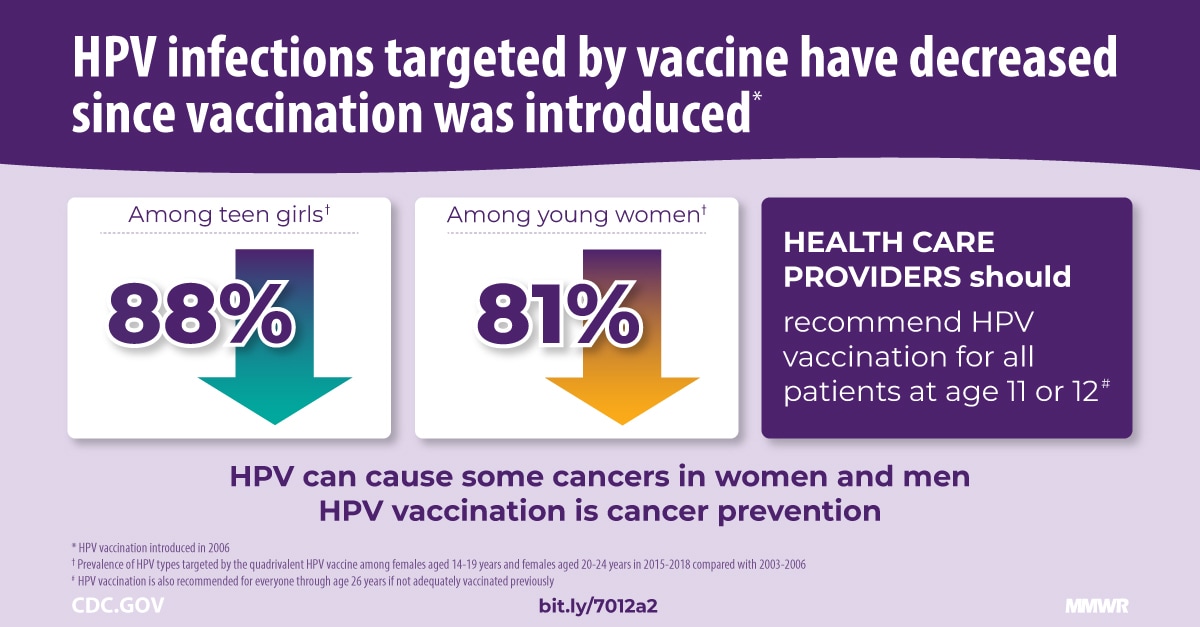
Global Impact on Health Outcomes
The widespread adoption of HPV vaccination programs has demonstrably reduced the incidence of HPV-related cancers and genital warts. Studies have shown substantial reductions in precancerous cervical lesions and, importantly, in the incidence of cervical cancer itself in regions with robust vaccination campaigns. These results indicate the significant public health benefit of preventing HPV infection and its associated diseases.
Prevalence of HPV-Related Diseases by Region
The prevalence of HPV-related diseases varies significantly across different regions. Factors such as socioeconomic conditions, cultural norms, and access to healthcare play a crucial role in shaping these disparities. A detailed analysis of the prevalence of cervical cancer, anal cancer, and other HPV-related malignancies across various geographical areas is essential to understand the specific needs and priorities for targeted intervention strategies.
| Region | Prevalence of Cervical Cancer (per 100,000 women) | Prevalence of Other HPV-Related Cancers (per 100,000 population) |
|---|---|---|
| North America | Low | Low |
| Sub-Saharan Africa | High | Moderate |
| South Asia | Moderate | Moderate |
| Europe | Low | Low |
Note: Data in this table are illustrative and may vary based on specific studies and reporting methods.
Reduction in HPV-Related Cancers Following Vaccination Programs
Numerous studies have documented significant declines in HPV-related cancers following the introduction of vaccination programs. In regions where vaccination coverage is high, reductions in the incidence of cervical cancer have been particularly notable. These findings underscore the effectiveness of the vaccine in preventing these diseases and highlight the need for sustained vaccination efforts. For example, in Australia, where vaccination programs have been implemented extensively, there’s been a demonstrable decrease in cervical cancer cases among young women.
Challenges in Implementing HPV Vaccination Programs in Developing Countries
Implementing HPV vaccination programs in developing countries faces several challenges. Limited access to healthcare infrastructure, including vaccine storage and administration facilities, is a major obstacle. Furthermore, cultural and societal factors, such as concerns about the safety and efficacy of the vaccine or gender-specific norms, can hinder program uptake. Addressing these challenges requires targeted interventions, such as community outreach and education campaigns, to build trust and increase awareness about the benefits of HPV vaccination.
Role of International Organizations in Promoting HPV Vaccination Globally
International organizations, such as the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), play a crucial role in promoting HPV vaccination globally. These organizations provide technical support, funding, and advocacy to countries striving to implement effective vaccination programs. Their initiatives include the development of guidelines, the provision of resources, and the facilitation of collaborations between nations to share best practices.
For example, the WHO recommends HPV vaccination as a vital component of national immunization schedules, aiming for global coverage.
“Global collaboration and support are essential to achieving equitable access to HPV vaccination, reducing the burden of HPV-related diseases, and safeguarding public health.”
HPV Vaccination and Specific Populations
HPV vaccination is crucial for protecting diverse populations from the long-term health risks associated with HPV infection. Understanding the unique needs and considerations for different groups is vital for maximizing vaccination coverage and impact. This includes recognizing potential barriers, addressing concerns, and tailoring vaccination strategies to optimize outcomes.Tailoring vaccination strategies to specific populations requires careful consideration of various factors, including access to healthcare, cultural norms, and individual circumstances.
This approach aims to overcome potential obstacles and encourage vaccination uptake, ultimately contributing to the prevention of HPV-related diseases and cancers.
Adolescent and Young Adult Vaccination Considerations
The adolescent and young adult years are a critical period for HPV vaccination. This is often a time of increased independence and potential changes in social networks, making it important to provide clear and accessible information about the benefits of vaccination. Vaccination during this period can significantly reduce the risk of HPV-related cancers later in life. Educational campaigns and partnerships with schools and healthcare providers can help overcome potential barriers.
HPV Vaccination for Immunocompromised Individuals
Immunocompromised individuals may have varying responses to HPV vaccines. Factors such as the type and severity of the immune deficiency influence the effectiveness of the vaccine. Healthcare providers must evaluate individual circumstances and potentially adjust vaccination schedules or dosages. Close monitoring and communication with healthcare professionals are crucial.
Addressing Concerns and Misconceptions about HPV Vaccination
Addressing misconceptions and concerns surrounding HPV vaccination is essential for increasing vaccine uptake. These concerns can stem from misinformation or lack of understanding about the vaccine’s safety and effectiveness. Open communication and providing accurate information can dispel these concerns and promote informed decision-making.
Potential Impact of HPV Vaccination on Reducing Health Disparities
HPV vaccination has the potential to reduce health disparities by addressing disparities in access to healthcare, socioeconomic factors, and cultural norms. By targeting populations disproportionately affected by HPV-related diseases, vaccination strategies can help narrow the gap in health outcomes and improve overall public health. This can involve community outreach programs and targeted interventions.
Vaccination Recommendations for Specific Demographics
| Demographic | Vaccination Recommendations |
|---|---|
| Adolescents (ages 11-12) | Ideally administered as a two-dose series, ideally starting before sexual activity begins. |
| Young Adults (ages 13-26) | Recommended for those who have not yet received the vaccine or completed the series. |
| Immunocompromised Individuals | Requires careful evaluation of the individual’s immune status. Consultations with healthcare providers are essential. Vaccination schedules or dosages may need adjustments. |
| Adults (ages 27-45) | Vaccination may still be beneficial for some individuals, especially those with risk factors. Discussions with healthcare providers are recommended. |
Future Directions and Research
The journey of HPV vaccination continues, driven by ongoing research and a desire to improve outcomes. Future efforts aim to expand access, optimize efficacy, and address the complexities of HPV’s impact on diverse populations. This includes developing more targeted and effective vaccines, refining vaccination strategies, and understanding the long-term effects of existing programs.Further research into HPV vaccination will likely focus on areas like vaccine effectiveness against emerging HPV types, the potential for personalized vaccination schedules, and the long-term consequences of HPV infections in vaccinated individuals.
New and Improved HPV Vaccines
Current HPV vaccines primarily target the most prevalent oncogenic HPV types. However, new strains continue to emerge, requiring researchers to develop vaccines capable of broader coverage. This involves exploring novel vaccine platforms, including mRNA technology, which could offer greater flexibility and adaptability in combating evolving HPV strains. Researchers are also investigating the development of vaccines that target HPV’s precancerous lesions, potentially preventing progression to cervical cancer.
This includes the potential for therapeutic vaccines aimed at eliminating existing infections. One example of an innovative approach is using viral vectors to deliver HPV proteins, potentially boosting immune responses.
Emerging Trends in HPV Vaccination Strategies
Vaccination strategies are evolving to enhance uptake and address specific population needs. This includes community-based vaccination programs, tailored to specific demographics and cultural contexts. For instance, innovative strategies might leverage mobile health units or community health workers to improve access in remote or underserved areas. Another emerging trend is the integration of HPV vaccination into routine adolescent health services.
This integration aims to enhance convenience and reduce barriers to vaccination, potentially leading to higher vaccination rates.
Importance of Continued Monitoring and Evaluation
Long-term monitoring and evaluation of HPV vaccination programs are crucial to understanding their impact. This involves collecting data on vaccination rates, HPV prevalence, and cancer incidence in vaccinated populations. Data analysis allows researchers to assess the effectiveness of different vaccination strategies and identify any emerging issues. This crucial data also allows adjustments to vaccination strategies as needed.
For example, monitoring the impact of a newly implemented school-based HPV vaccination program will reveal its effectiveness and provide insights for improvement.
Potential Role of Personalized Medicine in HPV Vaccination
Personalized medicine has the potential to further optimize HPV vaccination strategies. Factors such as genetic predispositions, immune responses, and prior exposure to HPV may influence the effectiveness of vaccination. Researchers are investigating how to incorporate these factors into personalized vaccination schedules, potentially increasing the efficacy of vaccination and minimizing adverse effects. For example, genetic testing might reveal individuals with a higher risk of developing HPV-related cancers, allowing for more tailored vaccination approaches.
Misinformation and Vaccine Hesitancy: Vacuna Virus Papiloma Humano
Navigating the complexities of public health initiatives, particularly vaccine programs, often requires addressing concerns and misconceptions. The HPV vaccine, like any preventative measure, faces a range of anxieties and doubts, which, if left unaddressed, can hinder its effectiveness. This section delves into the common misinformation surrounding HPV vaccination and the strategies for fostering vaccine acceptance.
Common Misconceptions about HPV Vaccination
Misinformation surrounding HPV vaccination often stems from a lack of accurate and accessible information. These misconceptions can range from unsubstantiated fears about side effects to inaccurate interpretations of the vaccine’s purpose. Understanding these prevalent myths is crucial to effectively addressing vaccine hesitancy.
- Safety Concerns: One of the most prevalent concerns is the perceived safety of the HPV vaccine. Debunked claims of significant side effects, such as long-term health issues, or a link to specific illnesses, are frequently circulated online. These false narratives can be perpetuated by individuals with vested interests or by those lacking scientific understanding.
- Unnecessary Vaccination: Some individuals believe that the HPV vaccine is unnecessary, either due to misconceptions about the prevalence of HPV or a lack of understanding of its potential health consequences. This can be attributed to a lack of awareness of the significant impact of HPV infections and the potential for long-term health issues such as cervical cancer.
- Lack of Evidence for Efficacy: Some doubts persist regarding the vaccine’s effectiveness, fueled by unverified reports or anecdotal evidence. These claims frequently fail to consider the rigorous clinical trials that support the vaccine’s efficacy and the substantial body of scientific evidence.
Strategies to Address Vaccine Hesitancy
Addressing vaccine hesitancy requires a multifaceted approach, combining accurate information dissemination with empathetic communication. Building trust and transparency is crucial.
- Evidence-Based Communication: Presenting clear, evidence-based information about HPV, its associated risks, and the vaccine’s safety and efficacy is paramount. This approach should be complemented by credible sources and verifiable data, ensuring accuracy and addressing misinformation head-on.
- Community Engagement: Actively engaging with communities through town halls, community events, and partnerships with trusted community leaders can foster open dialogue and address concerns. This approach emphasizes transparency and provides opportunities for individuals to ask questions in a safe and supportive environment.
- Addressing Concerns Directly: Openly acknowledging and addressing concerns about vaccine safety, efficacy, and potential side effects in a factual and compassionate manner is critical. This approach emphasizes empathy and a willingness to listen and respond to concerns.
Role of Public Health Campaigns
Public health campaigns play a vital role in combating misinformation and promoting vaccine acceptance. These campaigns should employ a range of communication strategies to reach diverse audiences effectively.
- Targeted Messaging: Developing targeted messaging tailored to specific demographics and communities can enhance the campaign’s impact. This strategy considers the unique values and concerns of different groups.
- Multi-Channel Approach: Utilizing various channels for communication, including social media, print media, and community forums, can ensure broader reach and engagement. This approach should aim to leverage the power of different media platforms to connect with diverse audiences.
- Collaboration with Experts: Collaborating with medical professionals, researchers, and public health experts is crucial for ensuring the accuracy and credibility of information disseminated through these campaigns.
Effective Communication Strategies
Employing effective communication strategies is crucial for promoting HPV vaccination acceptance.
Getting the HPV vaccine is super important for preventing certain cancers. While we’re on the topic of health, have you seen Eric Adams’s stylish suits lately? His fashion choices are always a conversation starter, and you can check out his amazing suit game on this page dedicated to his outfits eric adams suits fashion. Regardless of what he wears, the HPV vaccine remains a critical preventative measure for overall health.
- Using Visual Aids: Utilizing clear and engaging visuals, such as infographics and videos, can make complex information more accessible and easier to understand.
- Emphasizing Personal Stories: Sharing personal stories of individuals who have benefited from the HPV vaccine can foster trust and empathy. This approach should focus on the positive impact of vaccination.
- Building Trust with Credible Sources: Using credible sources, such as the CDC, WHO, and reputable medical organizations, enhances the campaign’s credibility. This approach focuses on transparency and reliability.
Comparing Approaches to Addressing Hesitancy
Different approaches to addressing vaccine hesitancy have varying degrees of success. Evaluating their effectiveness is essential for developing comprehensive strategies.
- Direct Confrontation vs. Patient-Centered Approach: Directly challenging misinformation with evidence-based arguments can be effective in certain contexts. Conversely, a patient-centered approach, which prioritizes listening to concerns and addressing anxieties, can foster trust and encourage vaccination.
- Fear Appeals vs. Benefit-Oriented Strategies: While fear appeals might prompt immediate action, benefit-oriented strategies, which highlight the positive impacts of vaccination, often lead to more sustainable behavioral changes.
Final Wrap-Up
In conclusion, vaccination against the human papillomavirus (HPV) is a powerful tool in preventing a variety of cancers and health problems. By understanding the science, the importance of timely vaccination, and the strategies for addressing vaccine hesitancy, we can collectively work towards a healthier future, free from the devastating impact of HPV-related illnesses. The ongoing research and development in this area are promising, paving the way for even more effective and accessible solutions in the years to come.
Questions Often Asked
What are the most common side effects of the HPV vaccine?
Common side effects include pain, redness, and swelling at the injection site, fever, and fatigue. These are usually mild and temporary.
Is the HPV vaccine safe for pregnant women?
The HPV vaccine is generally considered safe for pregnant women. However, it’s best to consult with a healthcare provider to determine the best course of action.
How does the HPV vaccine work?
The vaccine trains the body’s immune system to recognize and fight off HPV infection. This prevents the virus from causing infection and potential health problems.
What is the recommended age range for HPV vaccination?
The recommended age range for HPV vaccination typically begins in preteen years, often around 11 or 12, and can continue into adulthood. Consult your healthcare provider for personalized recommendations.

