
COVID Chronic Fatigue Syndrome A Deep Dive
Sindrome fatiga cronica covid is a complex condition that demands understanding. This blog post delves into the various facets of this post-COVID syndrome, exploring its symptoms, potential mechanisms, diagnosis, and treatment approaches. We’ll also examine the impact on quality of life and the ongoing research efforts to better comprehend and manage this debilitating condition.
The experience of post-COVID chronic fatigue syndrome varies significantly among individuals. While some experience only mild symptoms, others face a profound impact on daily life, necessitating a multifaceted approach to care.
Defining Chronic Fatigue Syndrome Post-COVID
Understanding post-COVID chronic fatigue syndrome (CFS) is crucial for proper diagnosis and management. This debilitating condition, characterized by persistent fatigue, can significantly impact a person’s daily life and overall well-being. Recognizing the specific symptoms and diagnostic criteria is essential for differentiating it from other conditions and ensuring appropriate treatment.
Defining Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome (CFS) is a complex medical condition primarily defined by persistent, debilitating fatigue that is not alleviated by rest. This fatigue significantly impacts daily activities and lasts for at least six months. It’s crucial to understand that the fatigue associated with CFS differs substantially from the tiredness one might experience after a demanding day. The exhaustion in CFS is profound and often accompanied by a range of other symptoms.
Furthermore, it’s essential to differentiate this from simply feeling tired or having a flu-like illness.
Diagnostic Criteria for CFS
The diagnostic criteria for CFS often involve a combination of factors. While there isn’t a single definitive test, the criteria generally include a persistent fatigue lasting for at least six months, along with the presence of other symptoms. Crucially, the fatigue must not be attributable to other medical conditions. Differentiating typical CFS from post-COVID CFS is also important.
Post-COVID CFS may manifest with similar symptoms, but the triggering event is known: COVID-19 infection. In both cases, a thorough medical evaluation is necessary to rule out other possible causes and establish an accurate diagnosis. This evaluation typically involves a detailed medical history, physical examination, and potentially various tests to exclude other conditions.
Prevalence and Impact of Post-COVID CFS
The prevalence of post-COVID CFS is still being studied and varies depending on the methodology and the specific populations investigated. Preliminary studies suggest that a significant portion of individuals who contract COVID-19 may experience persistent fatigue, potentially meeting the criteria for CFS. This has substantial implications for public health, as it indicates a potential long-term impact on individuals’ health and well-being.
The impact on various demographics, including age, gender, and pre-existing health conditions, needs further investigation. However, early evidence suggests that the condition may affect individuals of all ages and backgrounds.
Distinguishing CFS from Other Conditions
Differentiating CFS from other conditions that might present with similar symptoms is vital for accurate diagnosis and treatment. Conditions like fibromyalgia, other viral infections, and even some psychiatric disorders can mimic some symptoms of CFS. A key aspect is a comprehensive evaluation of the patient’s complete medical history, including pre-existing conditions, symptoms, and the duration of the symptoms.
This allows healthcare professionals to identify potential underlying causes and distinguish CFS from other conditions.
Comparison of Symptoms
| Condition | Symptoms |
|---|---|
| Chronic Fatigue Syndrome (CFS) | Persistent, debilitating fatigue lasting for at least six months, accompanied by other symptoms like muscle pain, cognitive difficulties, and sleep disturbances. |
| Fibromyalgia | Widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. Often associated with tenderness in specific areas. |
| Other Viral Infections | Fatigue, muscle pain, fever, headache, and other flu-like symptoms. The duration of these symptoms typically varies depending on the specific infection. |
This table provides a basic overview. The specific symptoms and their severity can vary considerably between individuals. It is important to remember that this is not an exhaustive list and other conditions may present similar symptoms. A thorough evaluation by a healthcare professional is necessary for accurate diagnosis.
Symptoms and Manifestations

The post-COVID chronic fatigue syndrome (CFS) experience is highly variable, making diagnosis challenging. Symptoms often overlap with those of traditional CFS, but there are also unique features emerging. Understanding the spectrum of physical, cognitive, and emotional symptoms is crucial for accurate diagnosis and effective management. This exploration will delineate the diverse manifestations of post-COVID CFS.
Physical Symptoms
Physical symptoms in post-COVID CFS often include persistent fatigue, which significantly impacts daily activities. This fatigue is frequently described as distinct from typical tiredness, and may not respond to rest. Other physical manifestations can include muscle pain (myalgia), headaches, and sleep disturbances. These symptoms are not always present, nor are they consistently the same across individuals.
- Fatigue: This is often the most prominent symptom, characterized by profound tiredness that doesn’t improve with rest and can significantly impact daily activities. Examples include difficulty concentrating, completing tasks, or even simple movements.
- Muscle Pain (Myalgia): Generalized muscle pain, often described as aching or soreness, is common. This pain can vary in intensity and location.
- Headaches: Headaches, including tension headaches and migraines, are reported frequently. These headaches may be associated with other symptoms or occur independently.
- Sleep Disturbances: Difficulty falling asleep, staying asleep, or experiencing restful sleep can be a significant issue. This can further exacerbate fatigue and cognitive impairment.
Cognitive Symptoms
Cognitive dysfunction is a hallmark of post-COVID CFS and often significantly impacts daily functioning. These symptoms can range from mild to severe, impacting a person’s ability to focus, remember, and learn.
- Brain Fog: A feeling of mental haziness or difficulty concentrating, often described as “brain fog,” is a common cognitive symptom. Individuals may struggle with tasks requiring focus and attention.
- Memory Problems: Short-term memory issues are frequently reported, affecting the ability to recall recent events or information. This can lead to difficulties in remembering appointments, conversations, or names.
- Difficulty with Executive Function: Challenges with planning, organizing, and completing tasks are common. This can impact daily routines, work performance, and personal relationships.
- Concentration Issues: Maintaining focus and attention is often difficult. This can affect learning, reading, and comprehension.
Emotional Symptoms
Emotional symptoms, while often overlooked, are a significant component of post-COVID CFS. These symptoms can include anxiety, depression, and irritability.
- Anxiety: Feelings of worry, fear, and nervousness can be prominent. This can be triggered by daily stressors or occur spontaneously.
- Depression: Symptoms of sadness, hopelessness, and loss of interest in activities can manifest. This can be related to the limitations imposed by the condition.
- Irritability: Increased sensitivity to stimuli and emotional outbursts are possible. This can be challenging for the individual and their relationships.
Symptom Variability
The severity and combination of symptoms vary significantly between individuals with post-COVID CFS. Some individuals may experience predominantly physical symptoms, while others may be more affected by cognitive or emotional symptoms. This variability highlights the need for personalized care and assessment.
Symptom Frequency Table
| Symptom Category | Common Symptoms | Frequency (Estimated) |
|---|---|---|
| Physical | Fatigue, Myalgia, Headaches, Sleep Disturbances | High (Often reported) |
| Cognitive | Brain Fog, Memory Problems, Executive Dysfunction, Concentration Issues | High (Frequently reported) |
| Emotional | Anxiety, Depression, Irritability | Moderate (Reported in many cases) |
Note: Frequency estimations are based on reported cases and are not definitive clinical data. Individual experiences can vary widely.
Differences from Typical CFS
While post-COVID CFS shares some similarities with traditional CFS, there are subtle but important differences. Some research suggests a potential link to specific viral-related immune system responses or neurological changes after COVID-19 infection. This could contribute to the unique symptom presentation in post-COVID CFS cases.
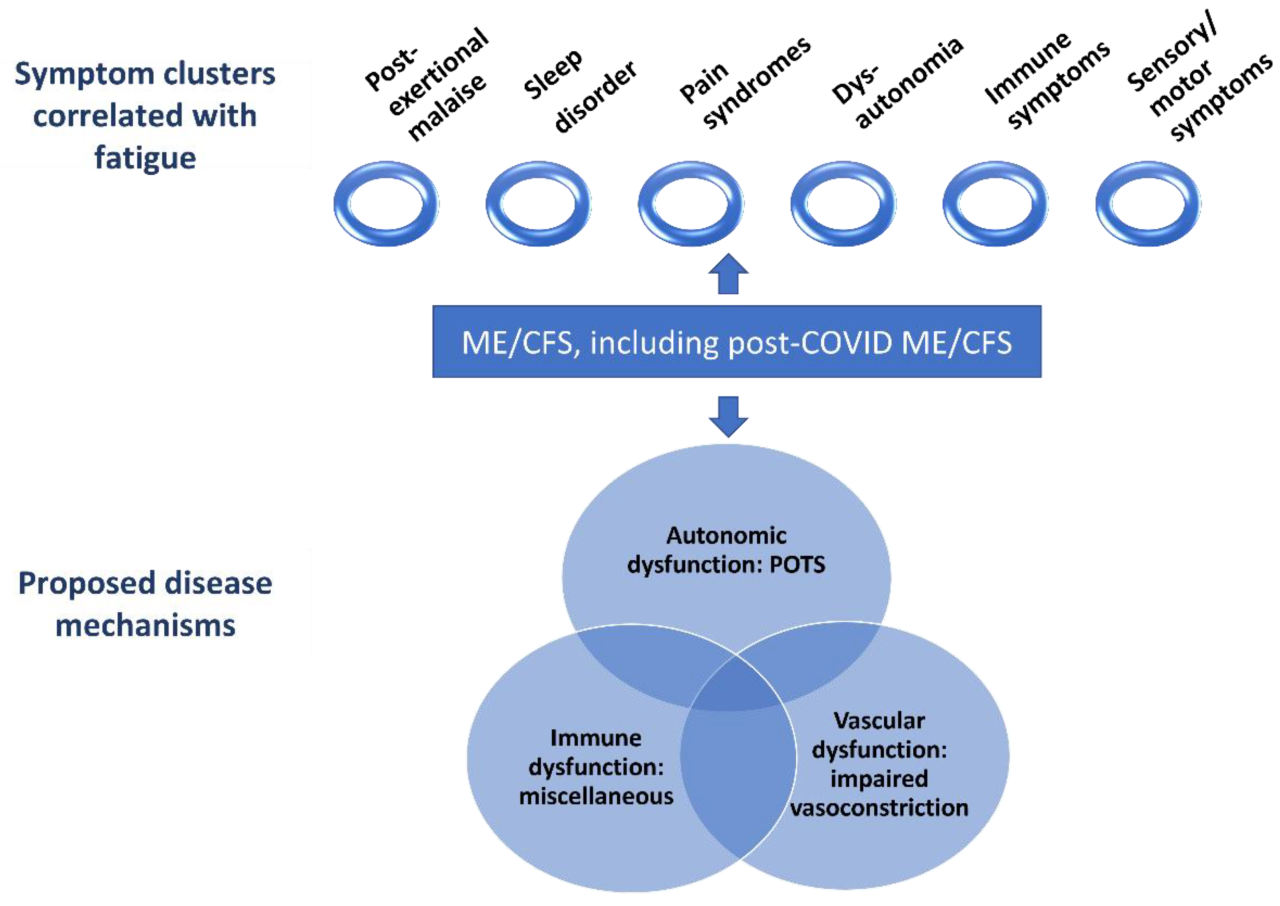
Potential Mechanisms and Contributing Factors
The link between COVID-19 infection and the development of Chronic Fatigue Syndrome (CFS) remains a complex and fascinating area of research. While the precise mechanisms are still being investigated, several potential pathways are emerging, highlighting the multifaceted nature of this condition. Understanding these potential mechanisms is crucial for developing effective diagnostic and treatment strategies.The complex interplay of inflammation, immune dysregulation, oxidative stress, pre-existing conditions, neurological implications, and psychological factors are all suspected to play a role in the development and persistence of post-COVID CFS.
This exploration delves into these potential mechanisms and contributing factors.
Potential Mechanisms Linking COVID-19 to CFS
Numerous mechanisms could explain how COVID-19 infection might contribute to the development of CFS. The viral infection itself can trigger a cascade of events that disrupt normal bodily functions, potentially leading to persistent symptoms. Understanding these pathways is crucial for developing effective treatments.
Role of Inflammation
Inflammation is a key component of the body’s response to infection. While a controlled inflammatory response is essential for fighting off pathogens, an overactive or prolonged inflammatory response can contribute to tissue damage and persistent symptoms. This heightened inflammation could potentially damage various organs and systems, potentially contributing to the development of CFS.
Ever feel completely wiped out, like you’ve been hit by a runaway train? That’s a common symptom of síndrome fatiga crónica COVID. Finding ways to cope with the lingering effects can be tough, but sometimes a bit of musical escapism can help. For instance, listening to broadway cast albums sweeney todd here can be a surprisingly effective distraction.
Ultimately, though, dealing with síndrome fatiga crónica COVID requires a multifaceted approach, combining rest, support, and sometimes, just a little bit of musical theater magic.
Immune Dysregulation
The immune system plays a crucial role in defending the body against pathogens. However, COVID-19 infection can disrupt the delicate balance of the immune response. This dysregulation can lead to a prolonged and uncontrolled immune reaction, which could contribute to persistent inflammation and the development of CFS. Examples of immune dysregulation include an overactive or underactive response to the virus, or an inability to properly clear the infection.
Oxidative Stress
Oxidative stress occurs when the body produces more free radicals than it can neutralize. This imbalance can damage cells and tissues, potentially contributing to various health problems. The COVID-19 infection may contribute to oxidative stress through the release of inflammatory cytokines and free radicals. This oxidative stress may play a role in the development of persistent symptoms, such as fatigue and muscle pain.
Impact of Prior Health Conditions and Pre-existing Vulnerabilities
Pre-existing health conditions, such as autoimmune disorders or chronic illnesses, may increase the susceptibility to developing CFS after a COVID-19 infection. Individuals with compromised immune systems or underlying conditions might have a harder time recovering from the infection, potentially leading to a more severe and prolonged inflammatory response. Genetic predisposition and other pre-existing vulnerabilities can also play a significant role.
Dealing with chronic fatigue syndrome post-COVID can be tough, especially when you’re trying to navigate life’s everyday challenges. Finding the right place to live is crucial for recovery, and the housing market near NYC is currently experiencing some interesting shifts. For those looking for apartments or homes in the area, checking out the latest trends in the housing market near NYC might be helpful.
Ultimately, finding a supportive and comfortable living situation is a key part of managing chronic fatigue syndrome.
Neurological Implications
COVID-19 has demonstrated the potential to affect the central nervous system. Neurological symptoms such as brain fog, headaches, and cognitive dysfunction have been reported in patients with post-COVID-19 syndrome. This raises the possibility of direct or indirect neurological damage contributing to the development of CFS. For example, studies have shown evidence of neuroinflammation in some patients.
Psychological Factors
Psychological factors can significantly impact an individual’s experience of illness and recovery. Stress, anxiety, and depression are common in individuals with chronic illnesses. These psychological factors can worsen symptoms and impede recovery. Furthermore, the experience of a severe illness like COVID-19 can be highly stressful, and this stress can contribute to the development of CFS.
Table of Potential Contributing Factors
| Contributing Factor | Mechanism | Examples |
|---|---|---|
| Inflammation | Overactive inflammatory response to infection | Muscle pain, joint pain, fever |
| Immune Dysregulation | Prolonged or uncontrolled immune response | Persistent fatigue, weakness |
| Oxidative Stress | Imbalance of free radicals and antioxidants | Headaches, brain fog, cognitive dysfunction |
| Prior Health Conditions | Increased susceptibility to prolonged illness | Autoimmune disorders, chronic respiratory illnesses |
| Neurological Implications | Direct or indirect damage to the central nervous system | Brain fog, cognitive impairment, headaches |
| Psychological Factors | Stress, anxiety, depression | Increased symptom severity, difficulty with recovery |
Diagnosis and Treatment Approaches
Navigating the complexities of post-COVID Chronic Fatigue Syndrome (CFS) requires a multifaceted approach, blending meticulous diagnostic tools with a personalized treatment plan. The challenges in diagnosis stem from the overlapping symptoms with other conditions, and the lack of a single definitive test for CFS. This necessitates a deep understanding of the individual’s medical history, symptom profile, and a careful exclusion of other potential causes.
Successful management relies on a collaborative effort between patients, healthcare providers, and therapists.
Challenges in Diagnosing Post-COVID CFS
The diagnostic process for post-COVID CFS is further complicated by the variability and often subtle nature of the symptoms. Patients may experience a constellation of symptoms that mirror other conditions, making it difficult to pinpoint the specific cause. The absence of a definitive biomarker further hinders accurate diagnosis, demanding a thorough evaluation of the patient’s complete medical history, including previous illnesses, lifestyle factors, and psychosocial stressors.
Symptoms such as fatigue, cognitive dysfunction, and sleep disturbances are common to multiple conditions, requiring careful differentiation.
Diagnostic Processes and Tools for CFS
The diagnostic process for CFS typically involves a comprehensive evaluation that considers multiple factors. This includes a detailed medical history, physical examination, and a thorough review of symptoms, including their duration, intensity, and patterns. Standardized questionnaires and scales, such as the Chalder Fatigue Scale and the Chronic Fatigue Syndrome Impact Scale, can assist in quantifying the severity and impact of the symptoms.
In some cases, laboratory tests may be used to rule out other conditions. These tests might include blood tests, urine analysis, or imaging studies, depending on the specific concerns raised by the patient’s history and symptoms. Furthermore, mental health assessments are crucial, as comorbid conditions like anxiety and depression can significantly influence the presentation of CFS.
Treatment Approaches for CFS
Effective treatment strategies for post-COVID CFS recognize the multifactorial nature of the condition. This necessitates a personalized approach that considers both conventional and alternative therapies. Conventional treatments frequently focus on symptom management, addressing fatigue, pain, and sleep disturbances. These can include medications, such as antidepressants or sleep aids, tailored to the individual’s needs and symptom profile. Physical therapy, cognitive behavioral therapy (CBT), and occupational therapy are also frequently utilized to improve functional capacity and address associated cognitive difficulties.
Alternative therapies, including acupuncture, massage therapy, and nutritional interventions, may also play a supporting role in managing symptoms.
Overview of Available Therapies and Efficacy
The efficacy of various treatment approaches for CFS varies significantly depending on the individual. Some patients may experience notable improvements with conventional therapies, while others might find greater benefit in integrating alternative approaches. A crucial element is the acknowledgment that there’s no one-size-fits-all solution. The effectiveness of a particular therapy often hinges on its alignment with the specific needs and characteristics of the individual patient.
Evidence suggests that a combination of therapies, often involving a multidisciplinary approach, yields the most promising outcomes. Success is usually measured not only by symptom reduction but also by an improvement in overall quality of life and functional capacity.
Importance of a Multidisciplinary Approach to Care
A multidisciplinary approach to care is crucial for managing post-COVID CFS effectively. This approach involves collaboration between physicians, therapists, and other healthcare professionals. A team-based approach allows for a holistic assessment of the patient’s needs, incorporating insights from various disciplines to create a personalized treatment plan. This plan addresses not only the physical symptoms but also the psychological and social aspects of the condition.
By fostering open communication and shared decision-making, patients can actively participate in their care, contributing to improved outcomes.
Summary of Treatment Options
| Treatment Option | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Conventional Medications (e.g., antidepressants, sleep aids) | May alleviate specific symptoms like fatigue and sleep disturbances. | Potential side effects, need for careful monitoring and adjustment of dosage. |
| Physical Therapy | Improves physical function, reduces pain, and enhances energy levels. | Requires commitment to regular sessions, and may not address all symptoms. |
| Cognitive Behavioral Therapy (CBT) | Helps manage negative thoughts and behaviors associated with CFS, improves coping mechanisms. | Requires active participation, and may not be suitable for all patients. |
| Alternative Therapies (e.g., acupuncture, massage) | May provide complementary support in symptom management. | Limited scientific evidence for effectiveness in some cases, and potential interactions with conventional treatments. |
Impact on Quality of Life and Societal Burden
Chronic Fatigue Syndrome (CFS) following COVID-19 infection presents a significant challenge, extending far beyond the initial illness. The lingering effects can profoundly impact various aspects of a person’s life, demanding attention to the broader societal burden and economic implications. This is not just a medical issue; it’s a complex interplay of physical, emotional, and social factors.The persistent fatigue, cognitive impairment, and other symptoms associated with post-COVID CFS significantly diminish an individual’s ability to participate in daily life, work, and social activities.
Understanding the scope of this impact is crucial for developing effective support systems and treatment strategies.
Impact on Personal Relationships, Sindrome fatiga cronica covid
Sustained fatigue and cognitive dysfunction can strain relationships with family and friends. Individuals may struggle to fulfill their roles as partners, parents, or children, leading to feelings of guilt, frustration, and isolation. The inability to participate in social activities, like gatherings or outings, can further contribute to feelings of social withdrawal and loneliness. This can impact communication, leading to misunderstandings and conflict.
Impact on Employment
The unpredictable nature of CFS often makes maintaining employment difficult. Fluctuations in energy levels, cognitive impairment, and the need for frequent rest periods can make consistent work attendance and productivity challenging. This can result in job loss, reduced work hours, or a shift to less demanding roles. Financial strain often accompanies job loss or reduced income, creating additional stress and compounding the impact on quality of life.
Chronic COVID fatigue syndrome (CFS) is a real struggle for many, impacting daily life in significant ways. It’s fascinating to see how political races, like the Winthrop Poll on Haley vs. Trump in South Carolina, highlighting current political dynamics , can still feel distant from the personal struggles of those dealing with long-term health issues. The ongoing challenges of CFS often feel isolating, and these broader political conversations can sometimes seem disconnected from the realities of the illness.
Still, it’s important to remember these individual battles are very real.
Impact on Social Activities
Post-COVID CFS often restricts participation in social activities. The physical and mental fatigue associated with the condition can make even simple social engagements overwhelming. This can lead to social isolation and a decline in social connections. The inability to engage in hobbies or activities that were previously enjoyed can significantly impact overall well-being.
Societal Burden
The societal burden of post-COVID CFS extends beyond individual suffering. The need for increased healthcare utilization, potential long-term care requirements, and lost productivity contribute to a substantial economic burden. This impacts healthcare systems, employers, and the overall economy. Supporting individuals with CFS requires significant resources, both financial and human.
Economic Implications
The economic implications of post-COVID CFS are substantial. Lost wages due to reduced work hours or job loss directly impact individuals’ financial well-being. Increased healthcare costs, including doctor visits, therapies, and medications, add to the financial strain. The burden on healthcare systems is also considerable, requiring increased resources for diagnosis, treatment, and management of this chronic condition.
This can strain existing resources and potentially limit access to care for other conditions.
Long-Term Consequences
Long-term consequences of post-COVID CFS can be profound. The persistent fatigue, cognitive dysfunction, and other symptoms can lead to a decreased quality of life, increased social isolation, and potential mental health issues, like depression and anxiety. The impact on physical health, including the development of secondary conditions, can also be significant.
Economic and Social Impact Table
| Impact Area | Description | Example |
|---|---|---|
| Personal Relationships | Strain on family and friend relationships due to fatigue and cognitive impairment. | Difficulty attending family events, decreased communication frequency. |
| Employment | Reduced work hours, job loss, or difficulty maintaining employment due to fluctuating energy levels and cognitive dysfunction. | Loss of income, need for reduced work hours, inability to perform job duties effectively. |
| Social Activities | Restriction in participation in social activities due to physical and mental fatigue. | Inability to attend social events, difficulty engaging in hobbies. |
| Societal Burden | Increased healthcare utilization, potential long-term care requirements, lost productivity. | Higher costs for healthcare, lost wages, impact on workforce productivity. |
| Economic Implications | Lost wages, increased healthcare costs, burden on healthcare systems. | Decreased income, higher medical expenses, strain on healthcare budgets. |
| Long-Term Consequences | Decreased quality of life, increased social isolation, potential mental health issues. | Persistent fatigue, depression, anxiety, and secondary physical conditions. |
Research and Future Directions

The journey to understanding and effectively managing post-COVID chronic fatigue syndrome (CFS) is paved with challenges, and research is critical to illuminating the path forward. Current knowledge gaps hinder the development of precise diagnostic tools and targeted treatments. Addressing these gaps requires a multifaceted approach, encompassing rigorous scientific investigation, innovative methodologies, and collaborative efforts from diverse stakeholders.
Current Gaps in Knowledge
Significant knowledge gaps exist regarding the specific mechanisms linking COVID-19 infection to the development of post-COVID CFS. The variability in symptom presentation and the complex interplay of factors contributing to the syndrome make it challenging to isolate causative factors. Moreover, the long-term effects of COVID-19 on the immune system, nervous system, and other bodily functions remain largely unexplored.
This lack of understanding complicates the development of effective diagnostic criteria and therapeutic interventions.
Key Areas of Ongoing Research
Ongoing research actively explores several crucial aspects of post-COVID CFS. Studies are investigating the role of inflammation, oxidative stress, and the dysfunction of the autonomic nervous system in the development and persistence of symptoms. The impact of viral persistence, immune dysregulation, and neuroinflammation is also being examined. Researchers are also delving into the psychological factors, such as anxiety and depression, which can exacerbate or contribute to the symptoms of post-COVID CFS.
Potential Future Research Directions
Future research should focus on developing more precise diagnostic tools, potentially utilizing biomarkers, such as specific immune cell profiles or neurochemical markers. Studies should also investigate the role of genetic predisposition and environmental factors in individual susceptibility to post-COVID CFS. Multi-center, longitudinal studies following patients over extended periods are essential to better understand the long-term prognosis and the natural course of the disease.
Furthermore, exploring the potential for personalized medicine approaches, tailoring treatment strategies based on individual patient profiles, holds immense promise.
Importance of Collaborative Research Efforts
Collaborative research efforts are vital for advancing our understanding of post-COVID CFS. Bringing together experts from diverse fields, including virology, immunology, neurology, psychology, and public health, can provide a holistic perspective. Cross-disciplinary collaborations can lead to innovative research methodologies and facilitate the development of more comprehensive treatment strategies. Sharing data and resources across institutions is essential to maximize the impact of research.
Need for Better Diagnostic Tools and Treatment Strategies
Current diagnostic criteria for post-COVID CFS often rely on symptom-based evaluations. Developing more objective and reliable diagnostic tools, including validated biomarkers, is crucial for accurate diagnosis and efficient treatment. Treatment strategies need to address the multifaceted nature of the syndrome, incorporating both pharmacological and non-pharmacological approaches. Addressing psychological factors, such as anxiety and depression, through appropriate therapies is essential for improving overall well-being and quality of life.
Current Research Projects
| Project Name | Focus Area |
|---|---|
| Impact of COVID-19 on Autonomic Nervous System | Investigating the role of autonomic dysfunction in symptom development and persistence. |
| Longitudinal Study of Post-COVID Fatigue | Following patients over time to assess the long-term prognosis and identify predictive factors. |
| Identification of Biomarkers for Post-COVID CFS | Searching for specific biological markers to aid in diagnosis and monitoring disease progression. |
| Psychosocial Factors in Post-COVID CFS | Examining the role of anxiety, depression, and other psychological factors in symptom severity and recovery. |
Illustrative Case Studies (Hypothetical)
Understanding post-COVID chronic fatigue syndrome (CFS) requires exploring real-world scenarios. These hypothetical case studies aim to illustrate the diverse experiences and challenges faced by individuals, highlighting the complexity of the condition and the nuances of diagnosis and treatment.These case studies are not intended to be definitive diagnoses but rather illustrative examples designed to promote a better understanding of post-COVID CFS.
Each case emphasizes the importance of a multidisciplinary approach to care and the long-term impact on the patient’s life.
Speaking of health struggles, chronic fatigue syndrome (CFS), often linked to COVID, is a real beast. It’s a complex issue, and while the Netanyahu hostage deal in Rafah is certainly a significant event, it’s important to remember that the long-term effects of COVID-19, such as netanyahu hostage deal rafah , can cause a wide range of health issues, including persistent fatigue and other debilitating symptoms.
This makes the ongoing research and support for those suffering from sindrome fatiga cronica covid even more crucial.
Case Study 1: Sarah
Sarah, a 35-year-old woman, experienced a mild COVID-19 infection three months prior. She initially recovered, but a few weeks later, she began experiencing persistent fatigue, headaches, and cognitive difficulties. These symptoms worsened over time, making it increasingly challenging to perform daily tasks. She felt a profound sense of exhaustion even after minimal exertion. Her memory and concentration were significantly impaired.
Sleep did not provide adequate rest.
Diagnostic Process and Treatment Plan
Sarah initially visited her primary care physician, who noted the persistent fatigue and associated symptoms. Further investigation involved blood tests to rule out other potential medical conditions. A detailed symptom evaluation, including questionnaires assessing fatigue severity and cognitive function, was crucial. Given the persistent and debilitating nature of the symptoms, a referral to a specialist in chronic fatigue syndrome was recommended.
The specialist conducted a comprehensive assessment, considering the patient’s medical history, symptoms, and the timeline of events following the COVID-19 infection. A diagnosis of post-COVID CFS was made after careful consideration and exclusion of other possible conditions.The treatment plan was multi-faceted. It included medication to manage pain and other symptoms, cognitive behavioral therapy (CBT) to address emotional and behavioral aspects of the condition, and graded exercise therapy (GET) to improve physical capacity.
Impact on Daily Life
Before the onset of symptoms, Sarah was a highly active individual, involved in numerous social activities and holding a demanding job. Post-COVID CFS significantly impacted her daily life. She had to reduce her work hours and eventually leave her job due to the severity of her symptoms. Social activities became extremely difficult to maintain. Her quality of life was severely compromised.
She experienced significant emotional distress and isolation, which were compounded by the challenges of navigating the healthcare system.
Patient’s Journey Through the Healthcare System
Sarah’s journey through the healthcare system was marked by delays and difficulties in obtaining a proper diagnosis. Initially, her symptoms were dismissed as stress-related or the lingering effects of the virus. It took several visits and consultations with different specialists to arrive at a definitive diagnosis. This delay significantly impacted her ability to access effective treatment and manage the condition’s effects on her daily life.
Chronic Fatigue Syndrome (CFS), often linked to COVID-19, is a complex health issue. Understanding the varying prevalence of health conditions across different regions, like the differences in demographics between red and blue states, might offer clues to potential contributing factors. For example, examining red blue states demographics could reveal correlations between certain socioeconomic factors and the incidence of CFS post-COVID.
Further research is needed to definitively connect these factors to the development of chronic fatigue syndrome.
The experience underscored the need for improved awareness and diagnostic protocols for post-COVID CFS.
End of Discussion: Sindrome Fatiga Cronica Covid
In conclusion, sindrome fatiga cronica covid presents a multifaceted challenge, demanding a comprehensive understanding of its various facets. From diagnosis to treatment, the journey is often complex, and support from healthcare professionals, family, and community is crucial. Continued research and collaboration are essential to improving the lives of those affected by this condition.
Key Questions Answered
What are some common cognitive symptoms associated with sindrome fatiga cronica covid?
Cognitive symptoms can include difficulty concentrating, memory problems, brain fog, and slowed thinking. These symptoms can significantly impact daily tasks and responsibilities.
How does sindrome fatiga cronica covid differ from other chronic fatigue syndromes?
While the core symptom of extreme fatigue is similar, sindrome fatiga cronica covid often presents with additional symptoms directly linked to a prior COVID-19 infection. There may also be differences in the severity and duration of symptoms.
What are some alternative treatment approaches for sindrome fatiga cronica covid?
Alternative therapies, such as acupuncture, massage, and mindfulness practices, are sometimes explored alongside conventional treatments. However, it’s crucial to discuss these options with a healthcare professional.
What is the role of psychological factors in sindrome fatiga cronica covid?
Psychological factors, such as stress, anxiety, and depression, can significantly impact the experience of sindrome fatiga cronica covid. A holistic approach to care often addresses these psychological factors in addition to physical symptoms.

