Alcohol Gut Health Microbiome A Deep Dive
Alcohol gut health microbiome: This intricate relationship between alcohol consumption, the gut’s delicate ecosystem, and overall health is a fascinating area of study. We’ll explore how different types of alcohol affect the gut microbiome, the impact on microbial composition, and how this complex interplay can lead to both short-term and long-term consequences for our well-being.
From the initial impact of a single drink to the long-term effects of chronic alcohol use, we’ll investigate the intricate mechanisms involved. We’ll also look at how the gut microbiome itself plays a role in alcohol metabolism and the potential for dietary strategies to support gut health recovery after alcohol consumption.
Introduction to Alcohol and Gut Health
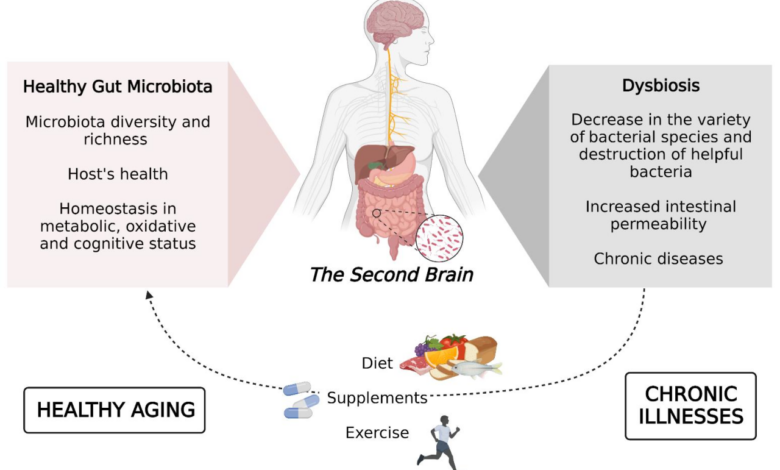
Alcohol consumption has a complex relationship with the gut microbiome, impacting its composition, diversity, and overall health. While moderate alcohol consumption might seem harmless, excessive or chronic intake can disrupt the delicate balance of gut bacteria, leading to various health consequences. This disruption is often manifested through inflammation, altered nutrient absorption, and even an increased susceptibility to certain diseases.
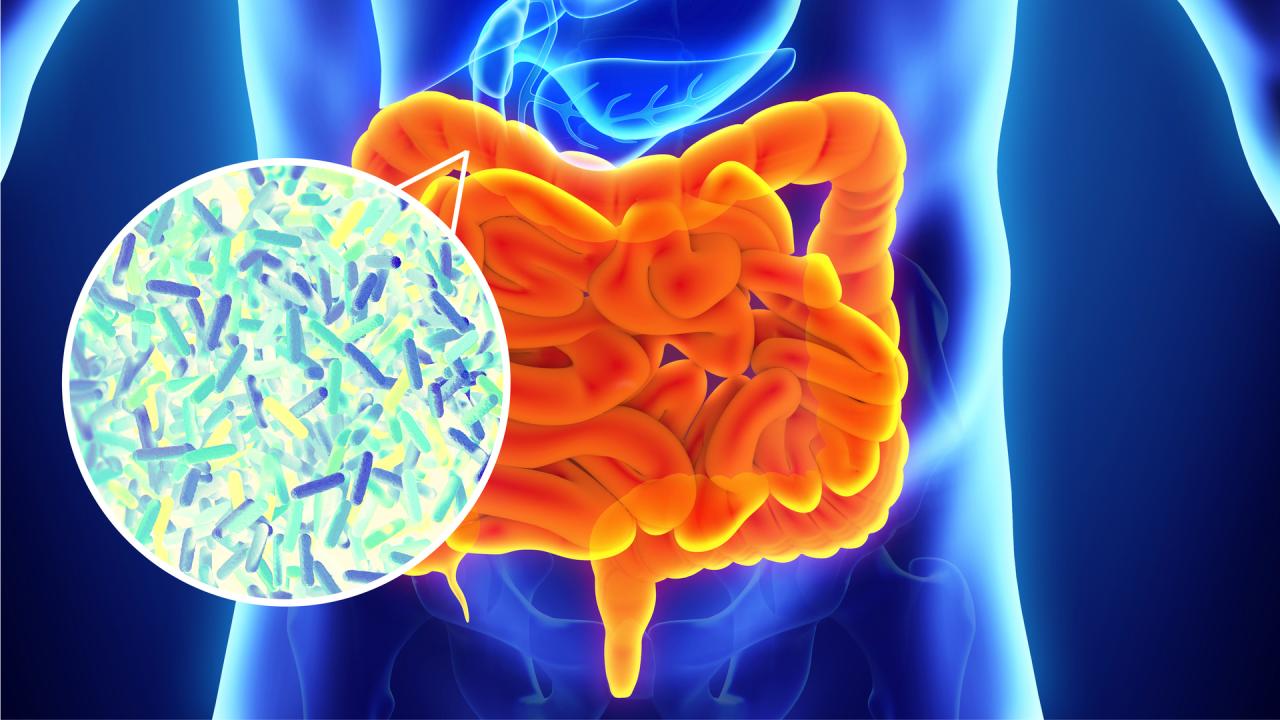
Understanding the mechanisms behind these interactions is crucial for developing strategies to mitigate the negative effects of alcohol on gut health.The human gut microbiome is a complex ecosystem containing trillions of microorganisms, including bacteria, fungi, and viruses. This intricate community plays a vital role in digestion, nutrient metabolism, and immune function. Alcohol, in various forms, can interfere with this delicate balance.
It can directly damage the gut lining, leading to inflammation and altered permeability. This altered permeability allows harmful substances to enter the bloodstream, potentially triggering a systemic inflammatory response.
Mechanisms of Alcohol’s Impact on the Gut Microbiome
Alcohol’s impact on the gut microbiome is multifaceted. It can alter the microbial composition by directly killing or inhibiting the growth of certain bacteria, while promoting the proliferation of others. This shift in microbial populations can lead to an imbalance, known as dysbiosis, impacting the overall function of the gut. Furthermore, alcohol can influence the production of metabolites by gut bacteria, affecting nutrient absorption and potentially triggering inflammatory responses.
Different Types of Alcoholic Beverages and Their Effects
The effects of different alcoholic beverages on the gut microbiome are not uniform. For example, the fermentation processes involved in wine production might contribute to different microbial communities compared to distilled spirits. The presence of polyphenols in wine, for instance, might have a protective effect, mitigating some of the negative impacts of alcohol.
Ever wondered how alcohol affects your gut health microbiome? It’s a complex relationship, and it’s more than just the occasional drink. Understanding how alcohol impacts the balance of good bacteria in your gut is crucial for overall well-being. For instance, if you’re curious about how parental surnames influence a child’s name, check out this interesting article on the topic of apellido bebe madre padre.
But let’s get back to the microbiome – consistent alcohol consumption can significantly disrupt this delicate ecosystem, potentially leading to various health issues.
Factors Influencing Individual Responses
Individual responses to alcohol’s impact on the gut microbiome are highly variable. Genetic predisposition, pre-existing gut health conditions, diet, and overall lifestyle choices all play significant roles in determining how the body processes and reacts to alcohol. An individual with a pre-existing gut condition, such as irritable bowel syndrome (IBS), might experience a more pronounced negative effect from alcohol consumption than someone with a healthy gut.
Comparison of Alcoholic Beverages and Gut Microbiome
| Alcoholic Beverage | Potential Effects on Gut Microbiome | Explanation |
|---|---|---|
| Wine (red) | Potentially protective effects due to polyphenols | Polyphenols in red wine may support beneficial gut bacteria and reduce inflammation. |
| Beer | Significant impact on gut microbiota composition | The fermentation process in beer production can lead to noticeable changes in gut bacteria populations. |
| Distilled Spirits (e.g., vodka, whiskey) | Potentially more disruptive effects | Distilled spirits lack the beneficial compounds found in some other alcoholic beverages. |
Impact of Alcohol on Gut Microbiome Composition
Alcohol consumption significantly alters the delicate balance of the gut microbiome, a complex community of bacteria, fungi, and archaea that play crucial roles in digestion, immunity, and overall health. This disruption can have long-lasting effects, contributing to various health issues, including inflammation and metabolic disorders. Understanding these alterations is vital for developing effective strategies to mitigate the negative consequences of excessive alcohol use.The gut microbiome is a dynamic ecosystem that responds to dietary changes, including the introduction of alcohol.
Ever wondered how alcohol impacts your gut health microbiome? It’s a complex relationship, and while a healthy gut is essential, excessive alcohol consumption can disrupt the delicate balance of good bacteria. Interestingly, a great example of dedication and resilience in the world of sports is evident in the career of Adrian Beltre, a Hall of Fame Texas Ranger Adrian Beltre Hall of Fame Texas Rangers.
His unwavering commitment to the game, just like the importance of maintaining a balanced microbiome, shows how dedication to health, both physical and internal, can truly impact success. So, let’s keep those good bacteria happy and thriving!
Alcohol acts as a substrate for some gut microbes, fostering their growth while potentially inhibiting the growth of others. This shift in microbial populations can impact the metabolic functions of the gut, leading to changes in nutrient absorption, toxin processing, and immune responses.
Specific Changes in Microbial Populations
Alcohol’s impact extends beyond simply affecting the total microbial count. It triggers specific changes in the composition of bacterial, fungal, and archaeal populations within the gut. For example, studies have observed an increase in certain opportunistic pathogens and a decrease in beneficial bacteria. These shifts in microbial diversity can have profound effects on the overall health of the gut and the body.
Key Bacterial Genera and Species Affected
Numerous bacterial genera and species are influenced by alcohol consumption. Firmicutes, Bacteroidetes, and Actinobacteria are among the most significantly affected groups. Specific species within these phyla, such as
- Bacteroides*,
- Prevotella*, and
- Lactobacillus*, demonstrate altered abundances. This change in bacterial communities can have a ripple effect on the metabolic processes within the gut.
Shifts in Microbial Metabolic Pathways
Alcohol metabolism by gut microbes generates byproducts that can impact the surrounding environment. These byproducts, in turn, can influence the metabolic pathways of other microbes. The activity of enzymes involved in carbohydrate, amino acid, and bile acid metabolism are often altered. For instance, increased ethanol metabolism by certain bacteria can lead to an accumulation of harmful metabolites.
Potential Consequences on Gut Health
These microbial shifts have various potential consequences for gut health. Disrupted microbial balance can increase inflammation in the gut lining, potentially leading to leaky gut syndrome. This can also impair the body’s ability to effectively regulate the immune system, making individuals more susceptible to various diseases. Furthermore, altered microbial metabolism can lead to nutrient malabsorption and impaired detoxification processes.
Impact of Chronic Alcohol Use on Gut Microbiome
| Bacterial Genus/Species | Relative Abundance (Chronic Alcohol Use) | Impact |
|---|---|---|
| *Bacteroides* | Decreased | Potentially reduced ability to ferment carbohydrates, impacting nutrient absorption. |
| *Prevotella* | Increased | Possible increase in the production of harmful metabolites. |
| *Lactobacillus* | Decreased | Reduced production of beneficial compounds and potential decrease in immune modulation. |
| *Escherichia* | Increased | Increased presence of opportunistic pathogens potentially contributing to gut inflammation. |
| *Clostridium* | Potentially Increased | Higher presence of species involved in harmful metabolic pathways. |
Note: The table illustrates potential changes; the specific effects can vary significantly depending on factors like individual genetic makeup, alcohol consumption patterns, and overall health status.
Role of the Gut Microbiome in Alcohol Metabolism
Our gut microbiome, a complex community of microorganisms residing in our digestive tract, plays a significant role in various bodily functions, including alcohol metabolism. This intricate relationship is influenced by the composition of the microbiome, and the microbial enzymes and pathways they utilize. Understanding these interactions is crucial for comprehending individual variations in alcohol tolerance and potential health risks associated with excessive alcohol consumption.The gut microbiome significantly impacts how our bodies process alcohol.
Certain microbial communities possess enzymes that can either enhance or hinder the breakdown of alcohol. These microbial-mediated processes, coupled with host-derived enzymes, contribute to the overall metabolism of ethanol. This intricate interplay between the microbiome and alcohol metabolism is not a static process; it can vary based on dietary factors, lifestyle choices, and even genetic predispositions.
Microbial Enzymes and Pathways in Alcohol Metabolism
The metabolism of ethanol primarily involves two major pathways: the alcohol dehydrogenase (ADH) pathway and the cytochrome P450 (CYP2E1) pathway. Both are crucial for converting ethanol into acetaldehyde, a toxic intermediate, which is then further oxidized to acetate. The gut microbiome can modulate the activity of these pathways through the production of various enzymes. For example, certain bacteria produce enzymes that can increase the efficiency of ADH, while others might increase the activity of CYP2E1.
This modulation can significantly affect the rate of alcohol metabolism.
Correlation between Microbial Communities and Alcohol Tolerance
Variations in gut microbial composition can correlate with individual differences in alcohol tolerance. Individuals with higher tolerance often possess microbial communities that efficiently metabolize ethanol. This efficient metabolism is often linked to higher abundance of specific bacterial species, like certain strains of
- Bacteroides* or
- Bifidobacterium*. Conversely, individuals with lower alcohol tolerance may have less efficient microbial populations for alcohol metabolism, leading to greater accumulation of acetaldehyde and a heightened risk of adverse effects.
Comparison of Ethanol Oxidation Pathways and Byproducts
The ADH pathway primarily oxidizes ethanol to acetaldehyde, which is further metabolized to acetate. The CYP2E1 pathway, though less significant in most cases, also contributes to ethanol oxidation, generating acetaldehyde as an intermediate. The difference lies in the rate of production and the potential impact on the body. High acetaldehyde levels are linked to negative health effects, including nausea, headaches, and flushing.
The specific microbial pathways involved in ethanol oxidation and the resulting byproducts significantly impact the overall metabolic burden on the body.
Diagram of Gut Microbiome-Alcohol Metabolism Interaction
[Imagine a diagram here depicting the interaction between the gut microbiome and alcohol metabolism. The diagram would show various bacterial species (e.g.,
- Bacteroides*,
- Firmicutes*,
- Fusobacterium*), their corresponding enzymes (ADH, CYP2E1), and the pathways of ethanol oxidation. Arrows would indicate the direction of ethanol metabolism, and the products generated (acetaldehyde, acetate) would be labeled. The diagram would also highlight the potential influence of different microbial communities on the rate of alcohol metabolism.]
The diagram would clearly illustrate how different microbial communities influence the activity of ADH and CYP2E1 pathways. It would visually show the role of the gut microbiome in ethanol oxidation and the resulting production of acetaldehyde and acetate. Furthermore, the diagram would highlight how variations in microbial composition correlate with individual variations in alcohol tolerance.
Alcohol-Induced Gut Barrier Dysfunction: Alcohol Gut Health Microbiome
Excessive alcohol consumption can significantly disrupt the delicate balance of the gut microbiome and negatively impact the intestinal barrier, leading to a cascade of inflammatory responses. This compromised barrier allows harmful substances to enter the bloodstream, contributing to various health problems. Understanding the mechanisms behind this disruption is crucial for developing strategies to mitigate the detrimental effects of alcohol on gut health.
Mechanisms of Alcohol-Induced Barrier Damage
Alcohol exerts its damaging effects on the intestinal barrier through multiple mechanisms. Direct toxicity to the cells lining the intestines, impaired tight junction function, and reduced mucus production all contribute to increased intestinal permeability. This disruption allows bacterial products and toxins to leak into the bloodstream, triggering an inflammatory response.
Key Components of the Intestinal Barrier Affected by Alcohol
The intestinal barrier is a complex structure composed of several crucial elements. Alcohol’s impact on the gut barrier often targets these components. Epithelial cells, forming the lining of the intestines, are directly exposed to alcohol and suffer damage from its toxic effects. Tight junctions, the specialized protein complexes that regulate paracellular permeability, are weakened, leading to increased intestinal permeability.
Mucus layers, a crucial protective barrier against pathogens and toxins, are compromised by alcohol consumption, further exposing the gut to harmful substances.
Consequences of Gut Barrier Dysfunction on Inflammation and Permeability
Gut barrier dysfunction, a direct result of alcohol consumption, leads to increased intestinal permeability, allowing harmful substances to enter the bloodstream. This triggers a significant inflammatory response. The inflammatory mediators released in response to this increased permeability contribute to chronic inflammation, which can have systemic effects, impacting various organs and tissues throughout the body. This increased permeability also allows bacteria and their products to reach the immune system, exacerbating inflammation and contributing to chronic inflammatory conditions.
Inflammatory Responses Triggered by Alcohol-Induced Gut Damage
The compromised intestinal barrier, a result of alcohol consumption, triggers a complex inflammatory response. The body’s immune system recognizes the presence of these harmful substances and initiates an inflammatory cascade. This involves the release of cytokines, signaling molecules that orchestrate the inflammatory response. Chronic alcohol consumption leads to a sustained inflammatory state, which can damage various tissues and organs and increase the risk of developing chronic diseases.
The inflammatory response is a natural defense mechanism, but when prolonged, it can lead to tissue damage and long-term health problems.
Factors Contributing to Alcohol-Induced Gut Barrier Dysfunction
| Factor | Mechanism |
|---|---|
| Direct Toxicity | Alcohol directly damages the epithelial cells lining the intestines, disrupting their integrity and function. |
| Impaired Tight Junction Function | Alcohol disrupts the structure and function of tight junctions, leading to increased intestinal permeability. |
| Reduced Mucus Production | Alcohol reduces the production of mucus, a protective barrier against pathogens and toxins, increasing the vulnerability of the gut. |
| Oxidative Stress | Alcohol metabolism generates reactive oxygen species, contributing to oxidative stress and cellular damage. |
| Disrupted Microbiome Composition | Alcohol alters the composition and diversity of the gut microbiome, which can further compromise the gut barrier. |
Long-Term Effects of Alcohol on Gut Health
Chronic alcohol consumption significantly alters the delicate balance of the gut microbiome, leading to long-term consequences that extend beyond the digestive system. This disruption can trigger a cascade of inflammatory responses and metabolic imbalances, ultimately increasing the risk of various diseases. Understanding these intricate connections is crucial for developing preventative strategies and targeted interventions.The long-term impact of alcohol on gut health is not merely a matter of discomfort; it’s a significant factor in the development of serious health problems.
The altered gut microbiome, often referred to as gut dysbiosis, plays a pivotal role in these consequences. This altered environment creates a fertile ground for the development of diseases that can have debilitating effects on an individual’s overall well-being.
Long-Term Consequences of Chronic Alcohol Consumption on Gut Microbiome
Chronic alcohol abuse disrupts the gut microbiota composition, leading to a shift in the types and quantities of bacteria present. This imbalance, known as dysbiosis, is characterized by a decrease in beneficial bacteria and an increase in potentially harmful species. This shift in microbial populations can impact the gut’s ability to perform its crucial functions, including nutrient absorption, immune regulation, and barrier integrity.
Link Between Alcohol-Related Gut Dysbiosis and Disease Development
Alcohol-related gut dysbiosis is directly linked to the development of various diseases. The disruption in the gut microbiome’s delicate ecosystem can trigger inflammatory responses, impair nutrient absorption, and compromise the gut barrier, making individuals more susceptible to infections and other health issues. For example, studies have shown a correlation between gut dysbiosis and the increased risk of developing inflammatory bowel disease (IBD) and colorectal cancer in individuals with a history of chronic alcohol use.
The impact of alcohol on gut health and the microbiome is a fascinating area of study. While some research suggests moderate alcohol consumption might have a slight positive effect, excessive drinking is definitely detrimental. This is a complex topic, especially when considering how stories like the tragic tale of lovers in Auschwitz, Keren Blankfeld and József Debreczeni, found frozen in the cold crematorium , highlight the devastating effects of human suffering and conflict on the human body and mind, which in turn could affect gut health in a completely different way.
Ultimately, understanding the microbiome’s delicate balance is crucial for our overall well-being, whether it’s influenced by alcohol consumption or other factors.
Mechanisms of Altered Gut Microbiota in Alcohol-Related Diseases
Several mechanisms explain how an altered gut microbiota contributes to alcohol-related diseases. One key mechanism involves impaired gut barrier function. Chronic alcohol exposure can damage the intestinal lining, allowing harmful bacteria and toxins to enter the bloodstream, triggering systemic inflammation. Furthermore, the altered gut microbiota can influence the metabolism of alcohol, leading to the production of harmful metabolites that can cause further damage to the gut and other organs.
Comparison of Moderate and Heavy Alcohol Consumption on Gut Health
Moderate alcohol consumption, often defined as one drink per day for women and two drinks per day for men, may have a less pronounced effect on the gut microbiome compared to heavy alcohol consumption. However, even moderate alcohol intake can lead to some degree of microbial imbalance over time. Heavy alcohol use, characterized by excessive and prolonged consumption, significantly disrupts the gut microbiota, leading to more pronounced dysbiosis and an elevated risk of developing alcohol-related diseases.
Potential Diseases Linked to Chronic Alcohol Consumption and Altered Gut Microbiome
| Disease | Potential Mechanisms |
|---|---|
| Inflammatory Bowel Disease (IBD) | Chronic alcohol use can damage the gut lining, increasing inflammation and permeability, which can contribute to the development of IBD. |
| Colorectal Cancer | Alcohol-induced gut dysbiosis can create a pro-inflammatory environment, leading to chronic inflammation and DNA damage, increasing the risk of colorectal cancer. |
| Liver Cirrhosis | Altered gut microbiota can contribute to liver damage through the production of harmful metabolites and increased intestinal permeability, increasing the burden on the liver. |
| Cardiovascular Diseases | Alcohol-related gut dysbiosis can contribute to systemic inflammation, increasing the risk of cardiovascular diseases. |
| Nutritional Deficiencies | Disrupted gut microbiota can impair nutrient absorption, leading to deficiencies in essential vitamins and minerals. |
Dietary Strategies to Support Gut Health After Alcohol Consumption
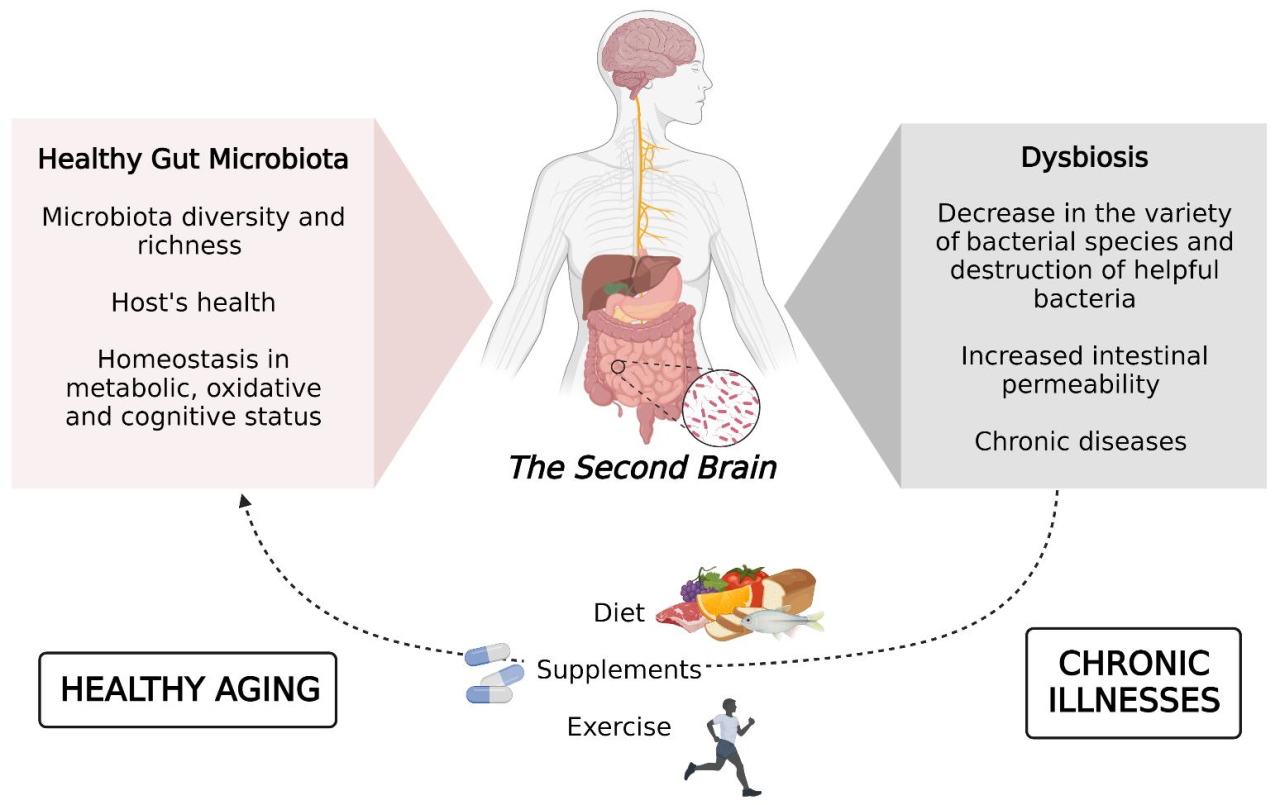
Recovering gut health after indulging in alcohol requires a strategic approach beyond just abstaining. The gut microbiome, a complex ecosystem of bacteria, fungi, and other microorganisms, plays a crucial role in digestion, immunity, and overall well-being. Alcohol can disrupt this delicate balance, leading to inflammation and damage to the gut lining. Nourishing the gut with the right foods and nutrients is essential for restoring its functionality and resilience.
Foods for Gut Restoration
A balanced diet rich in fiber, prebiotics, and probiotics can significantly aid in the recovery process. These nutrients support the growth of beneficial gut bacteria, promoting a healthy gut environment. Consuming a variety of fruits, vegetables, and whole grains provides the necessary fiber and vitamins that contribute to gut health.
Prebiotics: Feeding the Good Bacteria
Prebiotics are non-digestible food ingredients that selectively stimulate the growth and/or activity of beneficial bacteria in the colon. These beneficial bacteria produce important byproducts that are essential for gut health and overall well-being. Examples of prebiotic-rich foods include asparagus, onions, garlic, bananas, and leeks. Incorporating these foods into your diet can help to replenish and support the beneficial bacteria in your gut, helping it to recover from the effects of alcohol.
Probiotics: Introducing the Good Bacteria
Probiotics are live microorganisms that, when consumed in adequate amounts, confer a health benefit to the host. These microorganisms are beneficial to the gut because they compete with harmful bacteria for space and resources, preventing them from overgrowing. Yogurt, kefir, sauerkraut, and kimchi are all excellent sources of probiotics. These foods are rich in live bacteria and can help re-establish a healthy balance in the gut microbiome.
Studies have shown that consuming probiotic-rich foods can help improve gut health markers and reduce inflammation.
Hydration and Nutrition: Crucial for Gut Repair
Adequate hydration is essential for the entire body, including the gut. Dehydration can worsen gut inflammation and impair the gut barrier function. Drinking plenty of water throughout the day is crucial for overall gut health. Furthermore, a diet rich in vitamins and minerals, including vitamin C, vitamin D, and zinc, is vital for supporting the gut lining’s repair and recovery process.
I’ve been digging into the fascinating link between alcohol consumption and gut health microbiome lately. It’s a complex issue, and the latest results from the New Hampshire Democratic primary ( results new hampshire democratic primary ) got me thinking about the potential long-term effects of certain lifestyle choices on our overall well-being. The impact on our gut flora could be a hidden factor in these political results, and ultimately influencing our digestive systems and health in general.
It’s a reminder that our health is deeply connected to everything around us, even the political climate!
Foods Promoting Gut Health After Alcohol Consumption, Alcohol gut health microbiome
- Fruits and Vegetables: A wide array of colorful fruits and vegetables provide essential vitamins, minerals, and fiber, all of which support a healthy gut. Berries, leafy greens, and cruciferous vegetables are particularly beneficial.
- Whole Grains: Whole grains, like brown rice, quinoa, and oats, are excellent sources of fiber, promoting healthy digestion and supporting a balanced gut microbiome. They provide complex carbohydrates, which are essential for energy production and overall well-being.
- Legumes: Legumes, including beans, lentils, and chickpeas, are a good source of protein and fiber, contributing to a healthy gut environment. They are also packed with nutrients that support gut health.
- Fermented Foods: Yogurt, kefir, sauerkraut, kimchi, and miso are excellent sources of probiotics, which are live microorganisms that contribute to a healthy gut microbiome. These foods aid in restoring the balance of beneficial bacteria after alcohol consumption.
- Bone Broth: Bone broth is rich in collagen and minerals, which are essential for repairing the gut lining and supporting overall gut health. It is a great source of nutrients and can help soothe the digestive system.
Future Research Directions
Unraveling the intricate relationship between alcohol, the gut microbiome, and overall health requires further investigation. Current research provides a foundation, but many critical questions remain unanswered. Future studies must address the complex interplay of genetic predisposition, environmental factors, and individual lifestyle choices to develop personalized strategies for mitigating alcohol-related gut damage.Future research efforts will be instrumental in developing more targeted and effective interventions for those struggling with alcohol use disorders.
This involves investigating the potential of personalized approaches to support gut health, leveraging advanced technologies, and exploring novel therapeutic avenues such as probiotics and prebiotics.
The impact of alcohol on our gut health microbiome is a complex issue, with ongoing research. Recent studies highlight the potential disruption to beneficial bacteria. This isn’t just about individual health; it also connects to larger corporate influences, like the debate surrounding the Koch Chevron deference the Supreme Court has shown to these powerful companies. koch chevron deference supreme court Ultimately, understanding how these influences impact research and policy is crucial for bettering our overall understanding of alcohol’s effects on the gut microbiome.
Identifying Research Gaps in Alcohol-Gut Microbiome Interactions
The precise mechanisms by which alcohol disrupts the gut microbiome are not fully understood. Understanding the dynamic shifts in microbial populations over time and under varying alcohol consumption patterns is crucial. Further investigation is needed to identify the specific bacterial species or functional groups that are most vulnerable to alcohol-induced damage and the long-term consequences of these shifts.
Comparative studies are essential to evaluate the extent to which different types of alcohol affect the gut microbiome and to assess the role of genetic factors in influencing individual responses.
Exploring Probiotic and Prebiotic Interventions
Developing targeted probiotic or prebiotic interventions to support gut health in individuals with alcohol use disorders is a promising avenue for future research. Studies must evaluate the efficacy of specific probiotic strains in restoring beneficial gut bacteria, improving gut barrier function, and mitigating alcohol-induced inflammation. Similarly, research should investigate the impact of prebiotics on the composition and function of the gut microbiome, assessing their ability to modulate alcohol metabolism and reduce the risk of alcohol-related damage.
Determining the optimal dosage, administration schedule, and duration of these interventions will be key to successful outcomes.
Personalizing Strategies for Gut Health
Individual responses to alcohol vary significantly, highlighting the need for personalized strategies to support gut health in individuals with alcohol use disorders. Future studies should investigate the genetic and environmental factors influencing these diverse responses. This includes exploring the role of genetic polymorphisms related to alcohol metabolism, gut microbiota composition, and immune response. By understanding these individual variations, personalized dietary recommendations and therapeutic interventions can be tailored to optimize gut health outcomes.
Applying Advanced Technologies to Research
Metagenomics, a powerful technology capable of analyzing the entire genetic material of the gut microbiome, offers a unique opportunity to understand the complex relationships between alcohol, the gut microbiome, and health. These analyses can reveal the specific genes involved in alcohol metabolism, the presence of microbial toxins, and the changes in microbial communities associated with alcohol consumption. Combining metagenomics with other omics technologies, such as transcriptomics and proteomics, will provide a more comprehensive understanding of the molecular mechanisms involved.
Table of Research Gaps and Potential Research Directions
| Research Gap | Potential Research Direction |
|---|---|
| Precise mechanisms of alcohol-induced gut microbiome dysbiosis | Comparative studies of microbial communities in different alcohol consumption patterns, focusing on specific bacterial species and functional groups. |
| Efficacy of specific probiotics/prebiotics in mitigating alcohol-related gut damage | Clinical trials evaluating the impact of different probiotic strains and prebiotics on gut microbiota composition, barrier function, and alcohol metabolism. |
| Role of genetic factors in individual responses to alcohol | Genome-wide association studies to identify genetic polymorphisms influencing alcohol metabolism, gut microbiota composition, and immune response. |
| Application of advanced technologies in understanding complex mechanisms | Integration of metagenomics, transcriptomics, and proteomics to study the molecular interplay between alcohol, the gut microbiome, and health. |
Final Review
In conclusion, the alcohol gut health microbiome connection is a multifaceted area requiring further exploration. The intricate interplay between alcohol consumption, the gut microbiome, and potential health consequences is significant. Understanding these interactions is crucial for developing personalized strategies to support gut health in individuals with varying alcohol consumption patterns. The impact of diet and lifestyle choices is also highlighted, providing avenues for maintaining a healthy gut microbiome even after alcohol consumption.
User Queries
What are the short-term effects of alcohol on the gut microbiome?
Alcohol can temporarily disrupt the balance of gut bacteria, leading to a shift in microbial composition and potentially impacting digestion and nutrient absorption. This can manifest as bloating, discomfort, or diarrhea.
How does alcohol affect the intestinal barrier?
Alcohol can damage the intestinal lining, reducing its protective function. This damage can increase intestinal permeability, allowing harmful substances to enter the bloodstream and trigger inflammation.
Are there specific types of alcohol that affect the gut microbiome differently?
While more research is needed, some studies suggest that different types of alcoholic beverages might have varying impacts on gut microbial composition. For example, the type of alcohol (wine, beer, spirits) and its processing method may play a role.
Can prebiotics and probiotics help after alcohol consumption?
Preliminary evidence suggests that prebiotics and probiotics may play a role in restoring gut microbial balance after alcohol consumption. Further research is needed to determine the optimal types and dosages for optimal recovery.

